Chemical developed by Youzhong Guo launches as tool for cholesterol research and future drug discovery
A chemical designed by Youzhong Guo, Ph.D., an associate professor in the Department of Medicinal Chemistry, has been launched on the market. The chemical, called CHEAPS, maintains both the biochemical properties of cholesterol and the balance of hydrophobic – water-repellant – and hydrophilic – water-attracting – properties necessary for protein and cholesterol interaction research. Guo […]
Remembering renowned medicinal chemist, mentor and lyricist of VCU alma mater Lemont Kier
‘A stalwart’ in his field and the community, Kier developed pioneering scientific concepts while emphasizing student achievement – and embodying the spirit of ‘We Gather Here.’ Professor emeritus Lemont “Monty” B. Kier, Ph.D., whose nearly half-century at Virginia Commonwealth University included renowned contributions to the field of medicinal chemistry, mentoring hundreds of students and even […]
Expanding pharmacists’ role for patients with hypertension could prevent 15 million heart attacks and save $1.1 trillion over 30 years, VCU-led study finds
The study details how pharmacists’ ability to treat patients with hypertension could have a positive impact on both Americans’ quality of life and the U.S. health care system.
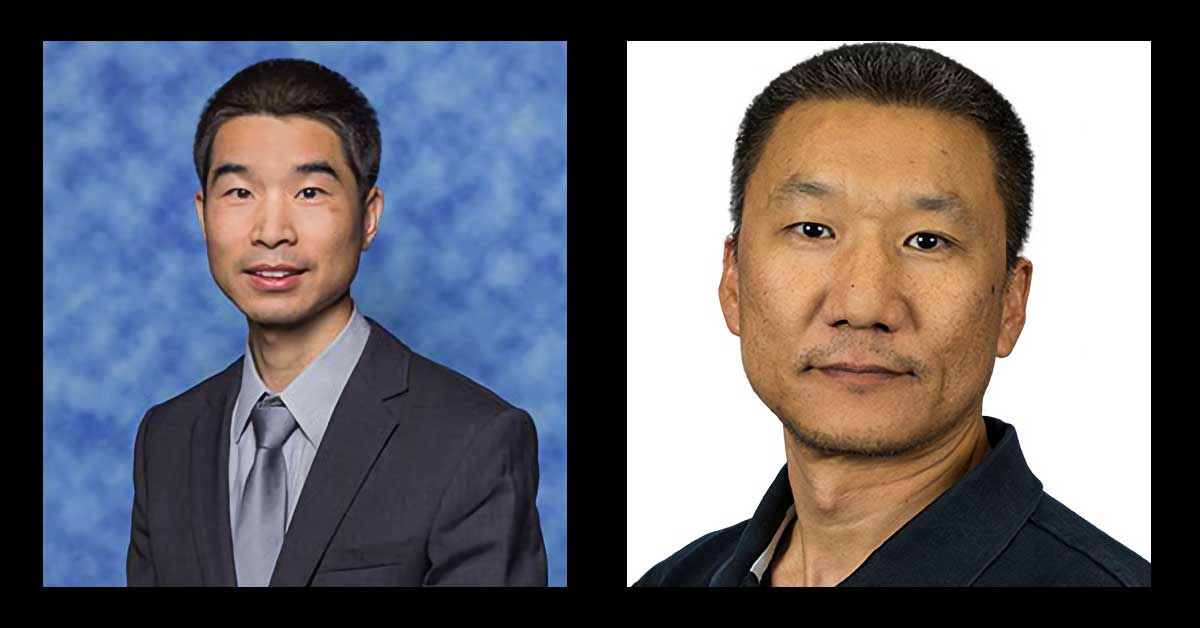
Two School of Pharmacy professors named first-ever NIRA scholars
A new VCU initiative highlights faculty members with demonstrated excellence in their academic discipline that not only elevate their national reputation, but enhance the profile of the entire university.
Department of Medicinal Chemistry featured in new SLAS Discover article
The VCU Department of Medicinal Chemistry in the School of Pharmacy has a long history of groundbreaking research that has been led by a series of distinguished scientists and department chairs, including Richard Glennon, Lemont Kier, Donald Abraham and Umesh Desai. Together, they and many other talented faculty members created a drug discovery ecosystem that […]
Pharmacy professors honored by VCU
Martin Safo, Ph.D., and Evan Sisson, Pharm.D., will be distinguished award recipients at this year's annual university faculty convocation.
Frankart selected as American Association of Colleges of Pharmacy ALFP fellow
The Academic Leadership Fellows Program (ALFP) is an initiative of the American Association of Colleges of Pharmacy (AACP). Dr. Laura Frankart has been selected as an American Association of Colleges of Pharmacy ALFP fellow in the 2023-2024 cohort. The Academic Leadership Fellows Program (ALFP) is designed to develop and support leaders in the Academy that […]
In a joyous ceremony, Class of 2023 wraps up “tumultuous” four years
Greg WeatherfordVCU School of Pharmacy More than 500 family members, friends and loved ones joined faculty and staff of VCU School of Pharmacy to celebrate the 2023 Hooding and Diploma Ceremony on a bright and sunny May day. [Note: Full list of awards can be found below.] “Health care is starving for leaders — in the […]
Circular mRNA may improve treatments
SoP researchers are changing the shape of the fight against COVID, cancer and more. Although they’ve been effective at preventing the virus, the VCU School of Pharmacy’s Guizhi “Julian” Zhu, Ph.D., notes that mRNA molecules used in those vaccines still have room for improvement: Their linear shape makes them more susceptible to being broken down […]
Pharm.D. program accredited through 2031
The Accreditation Council for Pharmacy Education has renewed accreditation for the VCU School of Pharmacy’s doctor of pharmacy program for a full eight-year cycle, effective through June 2031. The School of Pharmacy’s Pharm.D. program is accredited by the Accreditation Council for Pharmacy Education, based in Chicago. The accreditation term granted for the doctor of pharmacy […]