Periodontics research news

When you see him, please congratulate Dr. Zhao Lin upon receiving his first R01 grant. The title is “Epigenetic Regulation of Periodontal Inflammation,” which is supported by the National Institute of Dental & Craniofacial Research of the NIH. He will evaluate the epigenetic changes in patients with periodontitis and test the therapeutic potential of a novel “epi” drug in preclinical studies. The total award is about $1.9M for 5 years including direct and indirect costs. Wonderful news, Dr. Lin!
The following updates were provided by Drs. Zhao Lin and Harvey Schenkein who summarize their current projects and future research goals.
Regenerative Medicine and Epigenetic Regulation Periodontitis
- by Zhao Lin, BDS, MS, MMSc, PhD
Periodontitis is a common inflammatory disease caused by gingival bacteria, leading to the destruction of the tooth supporting complex. The ability to target the uncontrolled, overly aggressive inflammation and regenerate the periodontal tissues remains a great challenge to clinicians. Our laboratory is exploring novel strategies to treat periodontitis. One of our studies focuses on mesenchymal stem cells (MSCs), which hold great promise in regenerative medicine. We are studying whether extracellular vesicles from MSCs, including exosomes and matrix vesicles, can modulate periodontal inflammation and stimulate tissue regeneration.
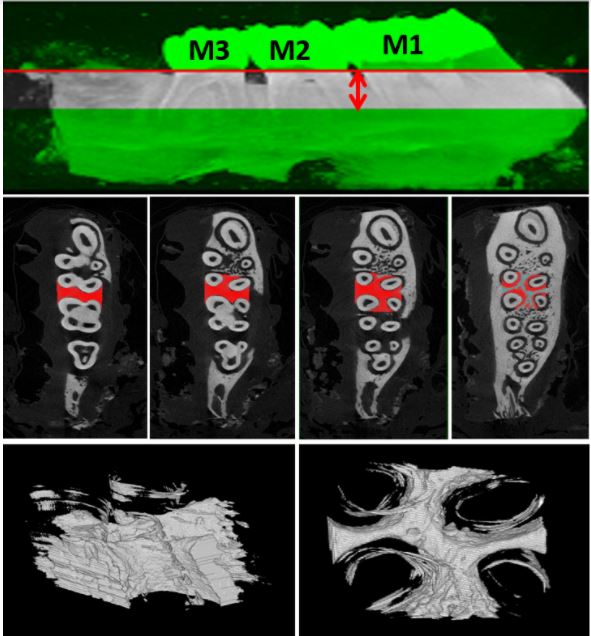
We are also interested in the epigenetic regulation of periodontitis. Epigenetic regulation, such as histone acetylation, is essential for inflammatory gene expression. A specific histone acetylation pattern is proposed in inflammatory diseases including periodontitis. Bromodomain and extraterminal domain (BET) proteins are the “readers” that mediate the epigenetic marks to the transcription machinery. BET inhibitors are an emerging class of epigenetic drugs for inflammatory diseases. To better understand epigenetic regulation in periodontitis and develop a novel therapeutic approach, we propose to 1) Identify the histone acetylation and BET protein expression profile in periodontitis patients; 2) Define the role of BET proteins in periodontal inflammation; 3) Determine if targeting histone acetylation by a selective BET inhibitor can ameliorate periodontal inflammation and alveolar bone loss in vivo. We are hoping that these studies will generate critical clinical data to support the importance of epigenetic regulation in the pathogenesis of periodontal disease and help us develop the first “epi” drug to treat the diseases.
Antiphospholipids and Periodontitis
- by Harvey A. Schenkein, D.D.S., PhD.
Our research laboratory is currently carrying out an NIH-funded project entitled “Antiphospholipids and Periodontitis”. Antiphospholipids are antibodies found in patients with an autoimmune disease called the Antiphospholipid Syndrome (APS), and which are frequently present in systemic lupus erythematosus (SLE). We noted several years ago that such patients suffer from thrombotic events, obstetrical complications such as spontaneous abortion, premature birth, preeclampsia and fetal growth retardation, as well as increased risk for cardiovascular problems. It seemed striking that the complications of APS were similar to some of the systemic conditions associated with periodontitis, and so we measured levels of anticardiolipin (aCL) antibodies in serum samples from periodontitis patients. We noted that about 20% of individuals with periodontitis have elevated levels of such antibodies. It had also been shown by other researchers that these antibodies can be produced by immunization of animals with certain bacteria and viruses (these microbes have components that were close enough in amino acid sequence to “mimic’ the human protein that reacts with anticardiolipin). We found that the periodontal pathogen Porphyromonas gingivalis also has such amino acid sequences. When we immunized mice with P. gingivalis we produced these antibodies, and when we administered the antibodies to pregnant mice, they exhibited fetal growth restriction and fetal loss.
We have been examining the properties of anticardiolipin antibodies that are found in periodontitis patients, as well as those induced by periodontal pathogens. We are finding that such antibodies exhibit several of the pathogenic properties observed for the autoantibodies seen in APS. For example, periodontitis patients with elevated levels of aCL also have elevated serum markers of vascular inflammation. They can stimulate immune cells to produce increased levels of inflammatory substances (cytokines), and they do so by activating the same cellular receptors. This is also true for the aCL that is induced by periodontal pathogens. Furthermore, the elevated levels of these antibodies persist even after scaling and root planing. These observations indicate that about 20% of periodontitis patients are chronically producing potentially pathogenic antibodies that appear in the systemic circulation. As these antibodies travel to tissues and organs distant from the oral cavity, they may increase systemic inflammatory responses and contribute to systemic pathology.
Categories Periodontics