Auxiliary Label: Antibiotic stewardship research in a community outpatient setting
By Victoria Hammond
Auxiliary Label Staff
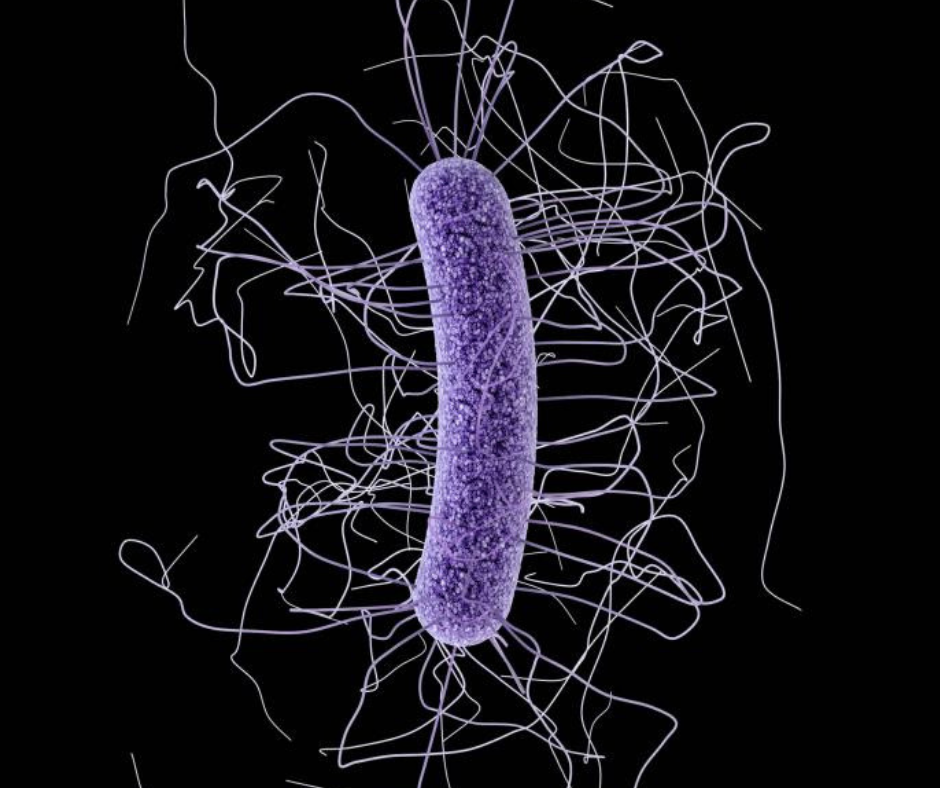
Antibiotic resistance — when bacteria are untreatable by current antibiotics — is a growing public health concern.
To reduce antibiotic resistance, prescribers use antibiotics only when necessary. In hospital settings, experts called antibiotic stewards monitor trends in resistance, prescribing, costs and adverse effects. Prescribing trends are compared to current treatment guidelines.
Stewards in an antibiotic stewardship have a goal to “enhance patient health outcomes, reducing resistance to antibiotics, and decreasing unnecessary costs,” according to the Society of Healthcare Epidemiology of America.
In 2015, about 269 million antibiotic prescriptions were dispensed in outpatient settings — at least 30 percent of which were unnecessary, according to the U.S. Centers for Disease Control. Unnecessary treatment of antibiotics can increase the risk of side effects or opportunistic infections such as C. difficile.
Settings with high volumes of antibiotics being prescribed would benefit from an antibiotic stewardship program to prevent side effects and opportunistic infection.
To improve patient outcomes in outpatient settings, VCU School of Pharmacy faculty members John Bucheit, Pharm.D., Teresa Salgado, M.Pharm., Ph.D., and Amy Pakyz, Pharm.D., Ph.D., have been implementing an antibiotic stewardship program in a free outpatient health clinic in the Richmond area. (They asked that the clinic’s name not be published.)
The faculty members’ first focus targets the prescribing trends of uncomplicated urinary-tract infections, or UTIs. Bucheit, Pakyz and Salgado are developing an antibiogram — a profile of antibiotic susceptibility for a specific practice site — based on prescribing trends from the past two years.
The antibiogram will provide information about which antibiotics are providing beneficial therapy to patients based on the clinic’s antibiotic susceptibility to resistant or nonresistant bacteria. This antibiogram will then be compared with current therapy guidelines to develop clinic specific guidelines for practitioners to use at the clinic. The project was made possible by a grant from the VCU School of Pharmacy’s Center for Pharmacy Practice Innovation.
“We are excited about this project to not only improve patient care at our clinic,” Bucheit said, “but also to provide an example for other outpatient offices interested in improving antibiotic prescribing for uncomplicated UTI.”
After the guideline is developed, Bucheit, Pakyz, Salgado and their team will educate the staff and reevaluate in a year.
The goal of this project is to provide prescriber education and improve patient health outcomes in a setting where high volumes of antibiotics are prescribed.
Auxiliary Label is a student-created blog examining pharmacy life, education and research at the VCU School of Pharmacy from a student perspective. It is overseen by Greg Weatherford, the school’s director of communications. Contact him here.
Categories Auxiliary Label, Community health, Faculty and staff news, Research, Student news
