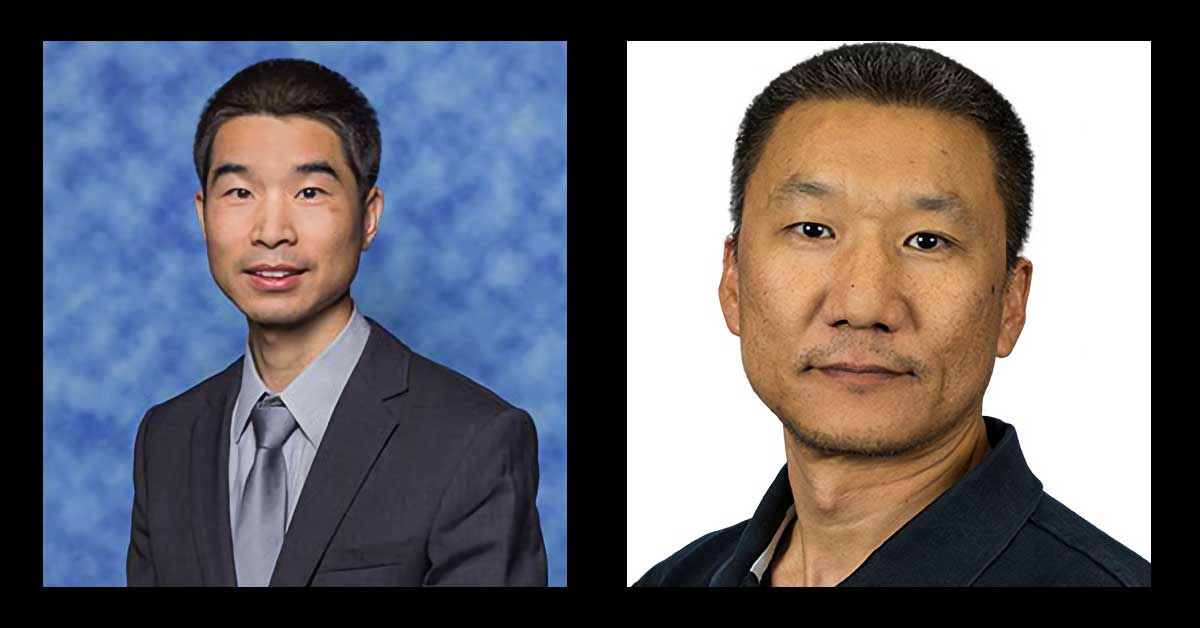
Two School of Pharmacy professors named first-ever NIRA scholars
A new VCU initiative highlights faculty members with demonstrated excellence in their academic discipline that not only elevate their national reputation, but enhance the profile of the entire university.
School of Pharmacy Research Day 2023
Research Day is for the entire VCU Pharmacy community and includes a trainee poster session (Pharm.D. and graduate students, and postdoctoral fellows), a showcase of SOP research and a keynote speaker. When Friday, October 27, 20238:00 a.m. to 1:30 p.m. Where Larrick Student Center900 Turpin St.Richmond, Virginia 23219 Agenda Time Agenda Item 8:00 a.m. – […]
Department of Medicinal Chemistry featured in new SLAS Discover article
The VCU Department of Medicinal Chemistry in the School of Pharmacy has a long history of groundbreaking research that has been led by a series of distinguished scientists and department chairs, including Richard Glennon, Lemont Kier, Donald Abraham and Umesh Desai. Together, they and many other talented faculty members created a drug discovery ecosystem that […]
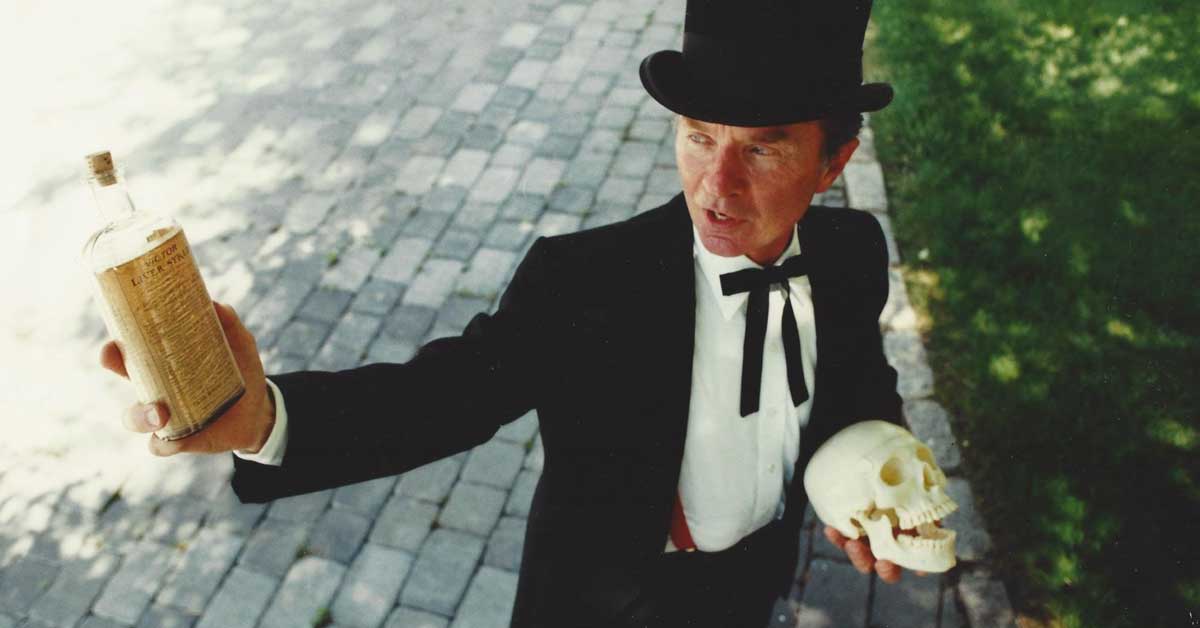
VCU School of Pharmacy community mourns loss of beloved alumnus Alvin J. Schalow
Esteemed alumnus Alvin J. Schalow, a prominent figure in the field of pharmacy, who left an indelible mark on the Virginia Commonwealth University School of Pharmacy and the Richmond community, passed away Aug. 20.
Faculty and staff awardees for 2023
Honorees were celebrated at the School of Pharmacy's first annual convocation in August.
Pharmacy professors honored by VCU
Martin Safo, Ph.D., and Evan Sisson, Pharm.D., will be distinguished award recipients at this year's annual university faculty convocation.
Frankart selected as American Association of Colleges of Pharmacy ALFP fellow
The Academic Leadership Fellows Program (ALFP) is an initiative of the American Association of Colleges of Pharmacy (AACP). Dr. Laura Frankart has been selected as an American Association of Colleges of Pharmacy ALFP fellow in the 2023-2024 cohort. The Academic Leadership Fellows Program (ALFP) is designed to develop and support leaders in the Academy that […]
Gawish named 2023 Healthcare Policy Fellow
VCU-based fellowship is the only one of its kind in the U.S. by Sydney Weber Wasem Gawish has been selected to be the American College of Clinical Pharmacy-American Society of Health-System Pharmacists-Virginia Commonwealth University Congressional Healthcare Policy Fellow for 2023-24. The 14-month fellowship, the only one of its kind in the nation, is based at […]
In a joyous ceremony, Class of 2023 wraps up “tumultuous” four years
Greg WeatherfordVCU School of Pharmacy More than 500 family members, friends and loved ones joined faculty and staff of VCU School of Pharmacy to celebrate the 2023 Hooding and Diploma Ceremony on a bright and sunny May day. [Note: Full list of awards can be found below.] “Health care is starving for leaders — in the […]
Graduate scholarship and research honored
School of Pharmacy’s 2023 Graduate Awards The School of Pharmacy’s annual Graduate Awards presentation took place at a celebratory luncheon at the Omni Hotel in downtown Richmond before a packed room of honorees, faculty, donors and alums. A keynote speech by alum Kamlesh Thakker traced his path from India to the School of Pharmacy and onward to tremendous success […]