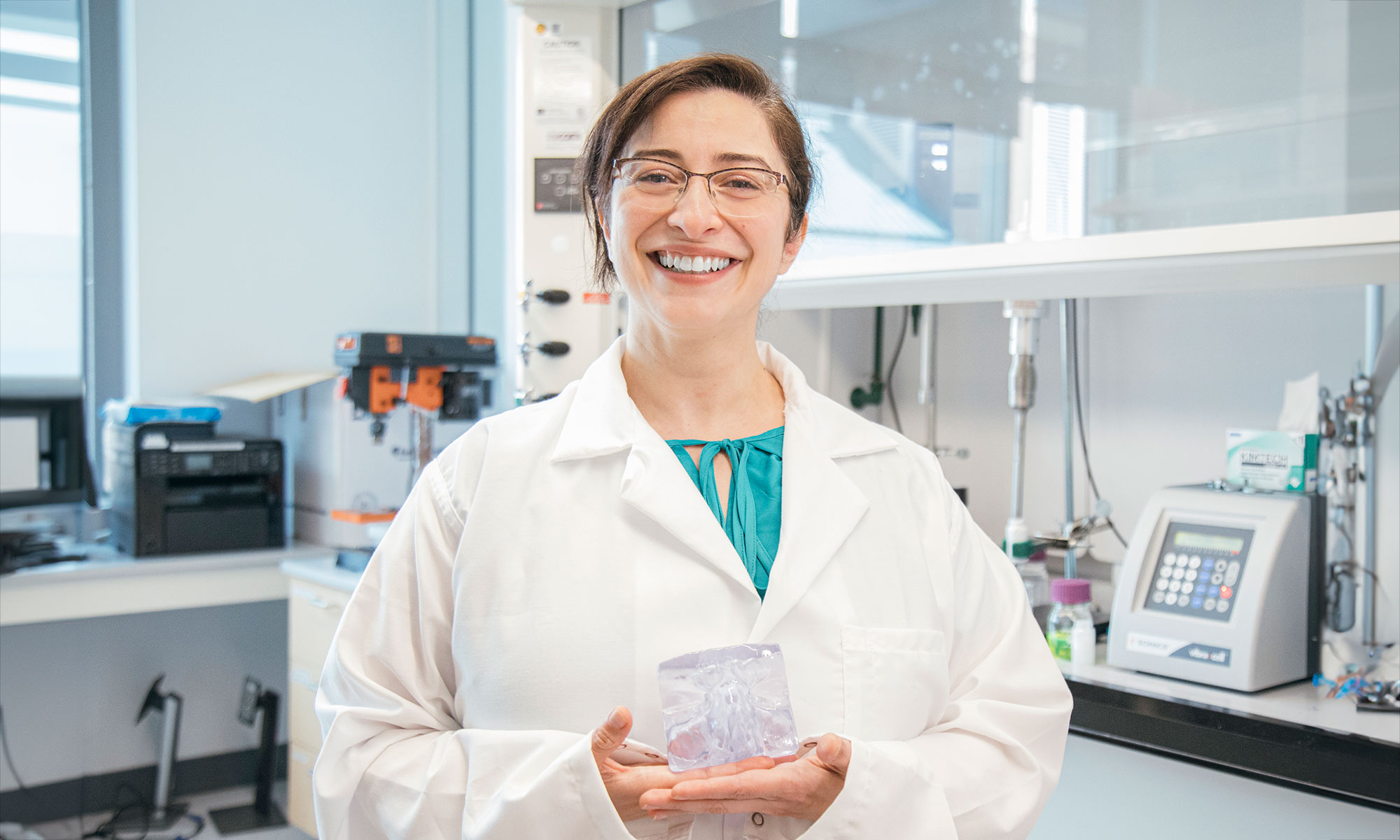
Demystifying aerosols: Laleh Golshahi, Ph.D., applies mechanical engineering principles to create personalized pharmaceutical treatments for patients
Self-described “aerosol nerd,” Laleh Golshahi, Ph.D., Engineering Foundation professor of mechanical and nuclear engineering, studies the human respiratory system to improve pharmaceutical aerosol technology. She is a pioneer in the development of personalized airway models for testing delivery systems like nebulizers, inhalers and nasal sprays.
“Mechanically, everyone’s respiratory system functions similarly,” Golshahi said. “Despite these fundamental similarities, there are many differences, especially when using the respiratory system to distribute medication. The smallest structural difference can alter how much medication needs to be applied. It can even result in the dose not reaching a patient at all. For example, in nebulizers and inhalers using the oral cavity for delivery, tongue position and other structural factors greatly impact effectiveness. Our goal is personalized medicine, tailoring aerosol delivery mechanisms to the patient and ensuring an effective dose is administered with each use.”
Golshahi’s Respiratory Aerosol Research and Education (RARE) lab uses CT or MRI scans to digitally render a patient’s nostril, nasal cavity, oral cavity, pharynx and larynx. The resultant model is a map for how to design an individualized aerosol delivery system to the lungs, nose or brain. Using additive manufacturing, a physical mockup is then connected to a machine that simulates breathing. This research recently received support from the TechTransfer and Ventures Commercialization Fund. Digital renders can also be tested without the need for 3D printing by employing computational fluid dynamics; however, these simulations cannot currently capture the full extent of information received from a practical experiment.
“For nasal sprays, respiration is different from nebulizers or inhalers,” Golshahi said. “By connecting the airway model to a breathing machine that simulates the lungs, we can find how much medication is trapped at different locations within the respiratory system and how much medication did not arrive at its intended location. A physical mockup of the patient’s respiratory system helps reduce the risk of improper treatment.”
Using an innovation Golshahi created, with the support of a multidisciplinary team of investigators, the patient’s nasal cavity model disassembles into several pieces. Investigating each piece tells researchers the path nasally-administered medication takes and how much material arrived at its intended destination.
Knowledge gained from these experiments has applications beyond aerosolized delivery of medication. Hospitals, for example, can use a respiratory model to calculate the gas required to sufficiently open a patient’s airways when oxygen is administered, so they breathe easily and without struggle.
With a training in mechanical engineering and a master’s degree in environmental engineering, Golshahi’s career did not start in pharmaceuticals. Her initial research focused on filtration systems for particulate matter, working on cyclone separators, which use centrifugal force to disperse fluid and particle elements, and packed bed filters, which trap suspended particles like dust or pollen, that improve air quality for manufacturing facilities and indoor spaces.
“Air quality was an issue in Tehran, where I received my undergraduate education,” said Golshahi. “Like any big city, I saw pollution and other environmental factors greatly affect people around me. I needed to understand how that impacts health. A close relative also struggled with chronic Central Nervous System (CNS) disease for many years, so I wanted my research to help families face challenges like this. I looked to solve disease-related problems with my engineering knowledge. For my Ph.D., I decided to approach filtration from a different angle. Our noses and throats are filters that protect the lungs, so looking at it from that perspective led my research to its current path investigating better forms of pharmaceutical drug delivery.”
Having worked on the mechanical aspects of aerosols, Golshahi expanded her research into the drug formulations used with nebulizers, inhalers and nasal sprays. Her team received a VCU Breakthroughs grant in 2022 to investigate a nose-to-brain delivery system to reach CNS through the nose.
Inhalers and nasal sprays belong to a special category of therapeutic products known as combination products. They incorporate devices or dispensers, drugs and/or biological compounds such as antibodies, vaccines, and gene cellular medicinal compounds into a single product. Since they cross traditional industry boundaries, like drugs, medical devices or biological compounds, separately, they give rise to unique challenges in development and regulatory considerations. This complexity comes from the drug or biological formulation interacting with the dispenser spray followed by the patient’s airway and tissues. Researchers must characterize the particulates throughout the process to ensure medication reaches its desired location, called the site of action.
“Our bodies are designed to protect us from material entering the respiratory system,” Golshahi said. “The nose-to-brain connection is a particularly complex pathway, which presents a challenge to the design of an effective medication and delivery system.”
Golshahi looks at viruses for inspiration. Their ability to bypass the respiratory system’s mucous layer and underlying tissue is exactly what her formulations need. By incorporating virus surface geometry and other characteristics into the design of medicinal particulates, they can pass through the junction between cells, circumventing mucus and tissue to arrive at the site of action.
Work done by Golshahi’s RARE lab is part of a larger group of aerosol specialists at VCU. Her postdoc with Michael Hindle, Ph.D., the Peter R. Byron Distinguished Professor in the VCU School of Pharmacy, brought Golshahi to the VCU College of Engineering, but the community of experts is what made her stay.
“VCU is a core for aerosol research,” Golshahi said. “We play a big role in the annual Respiratory Drug Delivery conference. The Greater Richmond Area is also home to a few companies that are very interested in aerosol and filtration technology. This all comes together at the Center for Pharmaceutical Engineering and Sciences, where researchers from many engineering disciplines gather to solve challenging questions related to drug delivery.”
The Center for Pharmaceutical Engineering and Sciences at VCU also hosts the United States’ only Ph.D. in pharmaceutical engineering. Golshahi is a mentor at the center along with many of her VCU aerosol research colleagues. In addition to the nose-to-brain delivery system for CNS-compromised patients, researchers in the RARE lab are also exploring nasal vaccine delivery, especially for pediatric use.
“We don’t fully understand the functionality of the nose-to-brain pathway,” Golshahi said. “Because of the unknowns, it’s an exciting area of study. The olfactory region is less than one percent of the nose, but has great promise. If we can figure out how to target it, nasal sprays will have even more applications, possibly treating things like depression and autism. It’s the future of medicine. Personalizing the treatment and delivery mechanisms we use lead to more effective dosing and, ultimately, healthier and happier patients.”
The Department of Mechanical and Nuclear Engineering provides undergraduate and graduate students with the opportunity to perform real-world research as soon as they enroll. From applying material science to additive manufacturing techniques to optimizing coolant systems for nuclear reactors and more, students gain understanding of many important engineering topics. Browse videos and recent news from the Department of Mechanical and Nuclear Engineering to discover how the College of Engineering at Virginia Commonwealth University prepares the next generation of scientists and engineers for the challenges of the future.
Categories Mechanical & Nuclear Engineering