Gut bacteria and health: VCU researcher leverages Wright Center resources to establish himself as leader in the field
Across the world, many years ago, doctors would prescribe unappealing concoctions of human and animal stool a treat a number of stomach ailments. And, in the last 10 years, clinical trials have begun to confirm why.
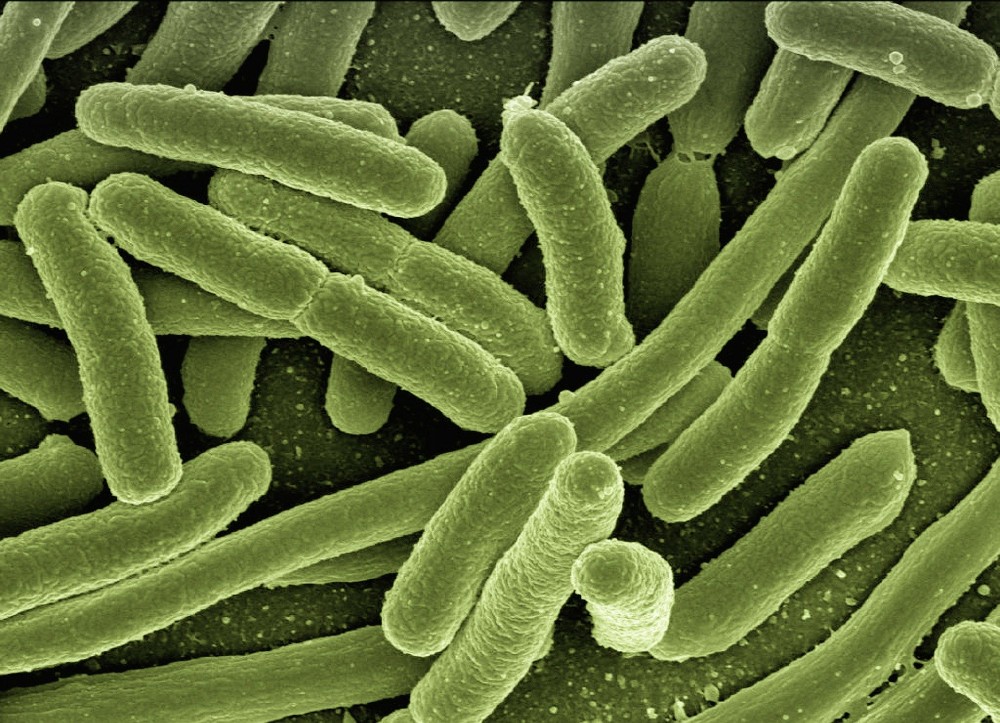
“There’s really a factory inside our bellies,” says Jasmohan Bajaj, M.D., a gastroenterologist and liver specialist at Virginia Commonwealth University. “Anything that we eat or drink, any medicines we take, when we get sick – the microbes are affected one way or the other. Either they are related to it, they process it, or they make us either resistant or prone to it.”

Bajaj is a major contributor to growing evidence that the unique collection of bacteria in our guts informs our health – sometimes in surprising ways. Fecal microbiota transplants – the newer, less unappealing version of that ancient treatment – are a big part of his research. And he’s leveraging the resources of the C. Kenneth and Dianne Wright Center for Clinical and Translational Research to accomplish his trials and study to become a leader in the field.
Working at a university with a Clinical and Translational Science Award (CTSA) from the National Institutes of Health, Bajaj has been awarded multiple grants that support his research into gut biomes and the uses of fecal transplants.
An R21 grant for 2017-18 helped Bajaj perform a randomized trial of fecal microbial transplant in patients with cirrhosis and hepatic encephalopathy.
This year he received another R21 grant to continue research into liver transplant outcomes, collaborating with a researcher another CTSA hub, the Columbia University Irving Institute for Clinical and Translational Research. The study will assess gut microbiota in patients with liver transplants in relation to their outcomes.
And he recently submitted an R01 to develop gut microbiota as a treatment for alcohol use disorder.
Bajaj also uses facilities maintained and funded by the Wright Center for his research. The Collaborative Advanced Research Imaging facility gives him access to a research-dedicated MRI scanner, which he’s using to analyze brain function in patients with cirrhosis before and after treating them with a gut-specific antibiotic.
A prolific summer of translational results
This summer, Bajaj published four articles showing the link between gut bacteria, cirrhosis and health.
A study into fecal microbiota transplantation in cirrhosis and hepatic encephalopathy showed that men and women respond differently to cirrhosis and to the medications that treat cirrhosis – and that may have to do with differences in gut microbiota. Results were published in the Journal of Hepatology and could lead to individualized care, based on someone’s biome.
Another study published in Gastroenterology analyzed the fecal microbiomes and their circulating products in hospitalized patients with cirrhosis and found they could identify cases that would soon result in death.
In July, Bajaj published a study comparing the death rates of patients with COVID-19 and cirrhosis with those experiencing just one of those diseases as part of a multi-center study. He found that patients with cirrhosis were more likely to die of COVID-19 than those without.
Finally, he completed and published a phase 1 study that found fecal microbiota transplants to be safe for patients with cirrhosis and showed promising results in reducing alcohol craving and consumption.
His research is helping show that the health outcomes associated with our unique gut microbiome go far beyond gastrointestinal diseases.
“The gut is one of the largest producers of neurotransmitters – the chemicals that allow your brain cells to talk to one another,” says Bajaj.
Doctors see the gut-brain connection in diseases like hepatic encephalopathy, a decline in brain function that occurs in people with chronic liver disease and often leaves them comatose or disabled. Previous research by Bajaj showed fecal microbiota transplants could improve brain function in those with the disease.
Making time to engage and inform
Through it all, Bajaj has found time to mentor junior faculty at VCU and spread awareness of his research to the public. He mentors Rising Scholars at the VCU School of Medicine. And he speaks often with local and national media outlets.
Most recently, he’s been interviewed by Healio, Medpage Today, and Richmond magazine about his promising phase 1 trial for fecal microbiota transplants as a treatment for alcohol use disorder.
Bajaj is keen to find something that works for patients with alcohol use disorder – and those experiencing the effects of prolonged alcohol use in the form of cirrhosis and hepatic encephalopathy. He notes that some doctors give up on people like his study participants, for whom other treatments have failed.
“People with alcohol use disorder are often discriminated against,” he says. “But it’s a disease like any other. There’s a genetic predisposition, and addictions may be promoted by those gut microbes.”
Categories Clinical Research, Clinical Trials, Facilities, Funding, Publications